The most effective nursing care integrates three crucial components: the best available research, clinical expertise, and an understanding of the patient’s unique needs and preferences. Known as evidence-based practice, this approach enables nurses to deliver patient-centered care that is backed by the most up-to-date science.
The origins of evidence-based practice in nursing care can be traced back to Florence Nightingale, the pioneer of modern nursing. Her research into the link between unsanitary conditions and poor health in the 19th century revolutionized nursing and paved the way for practices, such as handwashing and the sterilization of medical instruments, that are now standard in healthcare.
The application of evidence-based practice in healthcare has been shown to improve patient outcomes and patient satisfaction as well as reduce healthcare costs. For this reason, developing an in-depth understanding of evidence-based practice is crucial for nurses and nursing students. Nursing degree programs can help practitioners further enhance their knowledge and skills in evidence-based practice.
What Is Evidence-Based Practice in Nursing?
Providing holistic care to patients is a pillar of the nursing profession. Evidence-based practice is a reflection of this fundamental principle, calling on nurses to leverage their clinical experience, the latest scientific evidence, and their patients’ needs and values to deliver high-quality care.
Because healthcare is a constantly evolving field, nurses and other practitioners need to stay current on the latest research. Evidence-based practice in nursing ensures that care is grounded in proven methodologies, rather than personal beliefs or traditional methodologies.
Recognizing that evidence-based practice is an essential element of quality care, many healthcare organizations have established this approach as a professional standard for their nursing staff.
Selecting the Best Evidence
The ability to analyze and weigh available research evidence and determine its relevance to a patient’s unique circumstance is a critical part of a registered nurse’s job. According to the American Nurses Association (ANA), nurses should consider four levels of evidence when making clinical decisions:
Level A entails evidence from randomized, controlled trials. This level of evidence is considered the most reliable.
Level B is evidence from quality-designed control trials that are not randomized.
Level C evidence comes from expert opinion or a consensus viewpoint. This type of evidence comes into play when limited information is available about a condition.
Level ML (multilevel) incorporates evidence from more than one of the other levels. It is typically applied to complex cases.
Using these levels as a guide can help nurses determine how much stock to place in a particular study, report, or clinical practice standard when making decisions regarding patient care.
How to Implement Evidence-Based Practice in Nursing Care
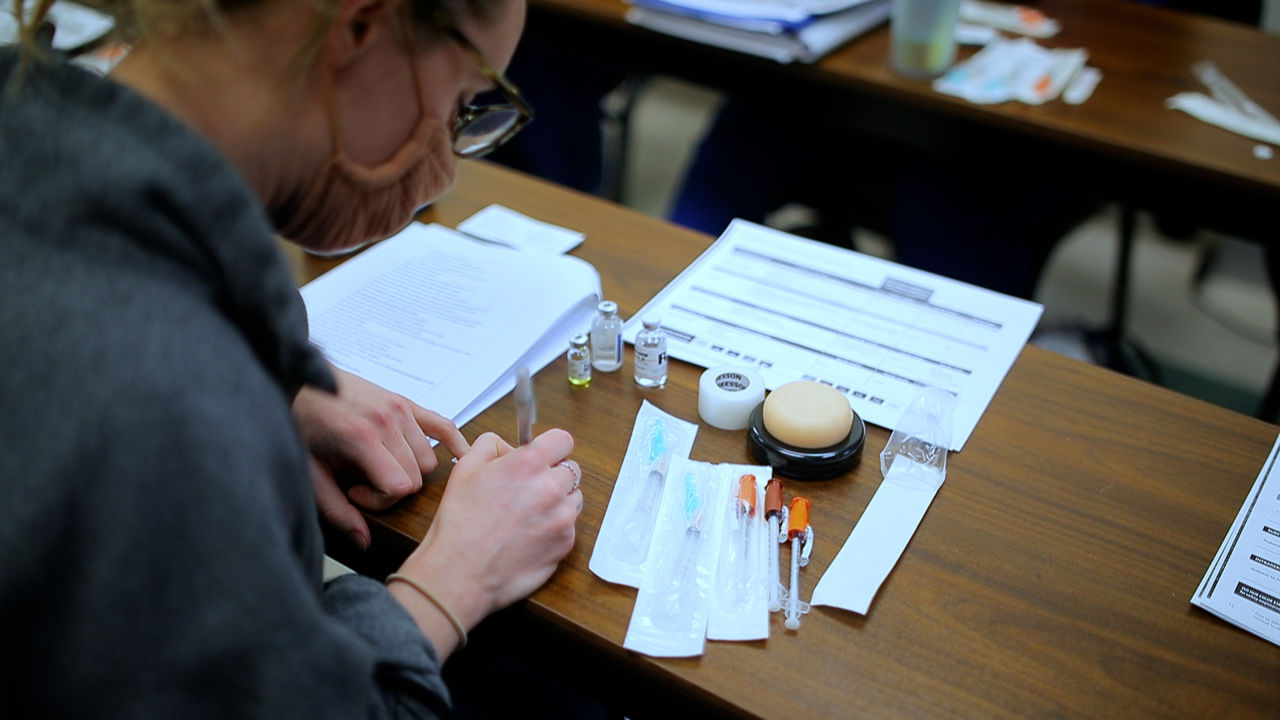
To effectively apply evidence-based interventions in their practice, nurses generally follow a five-step process, which serves to guide their patient care decisions:
Frame a clear, clinical question regarding the patient’s issue, and set a goal, such as improving a procedure, that helps their condition.
Gather evidence by searching relevant articles from legitimate sources.
Assess the evidence to determine its validity and relevance to the patient.
Apply the evidence to clinical practice, integrating individual clinical expertise and the patient’s unique needs.
Evaluate the outcomes to determine whether the intervention was effective.
Examples of Evidence-Based Practice in Nursing
Every day, nurses rely on research-backed evidence to provide superior care to their patients. This approach informs everything from how nurses treat patients with chronic conditions to how they interact with patients’ families. Common examples of evidence-based practice in nursing care include the following:
Implementation of disinfection protocols, such as handwashing and sterilization of instruments
Management of chronic conditions, such as angina or diabetes, using pharmacological and nonpharmacological interventions
Implementation of patient positioning guidelines to minimize the risk of injuries resulting from pressure
Use of oxygen use to assist with oxygen deficiency and organ failure in patients with chronic obstructive pulmonary disease (COPD)
Implementation of fall prevention practices, including the use of patient monitoring tools and an assessment of the risk of falls using the Morse Fall Scale (MFS)
An evidence-based approach can be applied outside of clinical contexts as well. For example, a nurse leader may use the latest research on nursing operations to implement a new staffing model to improve a unit’s efficiency.
Why Is Evidence-Based Practice in Nursing Important?
The application of evidence-based practice in nursing has numerous advantages, not least of which is the potential to improve patient outcomes. A 2023 scoping review published in Worldviews on Evidence-Based Nursing found that, in cases where clinicians used evidence-based practices, patient outcomes improved in nearly 90% of the cases. The studies included in the review measured a host of patient outcomes, such as length of stay, mortality, patient compliance/adherence, and readmission — all of which saw overwhelming improvement when evidence-based practices were used.
The other potential benefits of evidence-based practice include the following:
Promotes shared decision-making with patients, leading to greater patient satisfaction and adherence to treatment
Enhances nurse autonomy and confidence
Facilitates the incorporation of new technology into nursing practice
Helps nurses hone critical-thinking skills
Encourages lifelong learning
Contributes to the growth of nursing science
Evidence-based practice has also been shown to reduce healthcare costs by preventing complications and reducing readmission. The same Worldviews on Evidence-Based Nursing report revealed that healthcare organizations saw a positive return on investment 94% of the time when evidence-based practices were used.
Enhance Your Nursing Practice With a Bachelor of Science in Nursing or a Master of Science in Nursing
Understanding and applying research evidence to their professional practice is every nurse’s duty. This holistic approach ensures that patient care is backed by the latest science, leading to improved outcomes and reduced costs.
Registered nurses (RN) seeking a Bachelor of Science in Nursing (BSN) or a Master of Science in Nursing (MSN) can enhance their knowledge of evidence-based practice by enrolling at Denver College of Nursing. Our online RN to BSN and MSN programs — which are both accredited by the Commission on Collegiate Nursing Education (CCNE) — have been designed by working nurses for working nurses who want to further develop their skills and leadership abilities.
If you are an RN looking to take the next step in your career, find out how Denver College of Nursing can help you get there.
Recommended Readings
7 Nursing School Tips for Studying
How to Write a Winning Nursing Application Essay
What Is a BSN Completion Program and How Does It Work?